With the 2020 Olympics currently happening in Tokyo, Japan – doctor Alexandra Myers has been giving interviews to news publications and has been quoted in a number of articles. Read some of the Olympic coverage and get a doctors perspective from the articles and newspapers below.
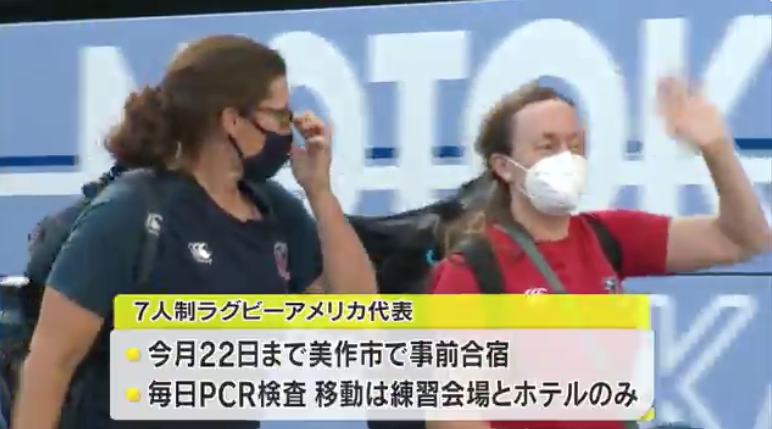
Tokyo Olympics USA Rugby Sevens arrive in Mimasaka with minimal welcome to prevent Covid infections
DOs at the Tokyo Olympics share the joys and challenges of working with world-class athletes
Get Olympic DOs’ advice for aspiring sports medicine docs and learn what it takes to care for elite athletes.
The DO spoke with Dr. Rao, Dr. Myers and Dr. Lally to get an inside scoop on the highs and lows of practicing sports medicine at the highest level. Following is an edited Q&A with answers from Dr. Myers.
What does the pre-Olympics prep looked like?
For rugby, athletes train at the Chula Vista Elite Athlete Training Center in Southern California. I practice in San Diego, so I see them on a regular basis.
Whenever they have injuries during training, or when they’re competing abroad, they come back and I see them here. In a given week, I’m seeing one or two players. So it’s a pretty close-contact situation.
I also cover their scrimmages. The men had Argentina in town recently, and the women had Brazil in town.

What should viewers watching your sport be looking for when they watch the Olympics?
Olympic rugby is a very quick game, so you have to pay attention. There’s no stoppage time. In football, when the ball is down on the ground, the play is over.
But in rugby, it’s continuous play until somebody gets a try, which is like a goal or touchdown. You have to keep watching the ball.
What are the common injuries you see in your sport?
In rugby, we see lots of broken hand bones, broken fingers and concussions. The big thing we worry about is spine injuries. We’ve had a couple this year, but they weren’t catastrophic. One of our athletes went through getting a cervical disc replacement and rehab and getting back into contact sports.
What advice would you give to medical students who would like to become team physicians for athletes competing at the Olympics one day?

I recommend shadowing a sports med physician and working with local sports teams. When I was in residency, I worked with one of our ER doctors who covered high school football. I took over the high school football coverage, and I had three years of high school football experience before I got into fellowship, which was super helpful.
You may have to recalibrate your income expectations. Sports medicine is not the highest paid specialty, and most of the cool jobs are actually volunteer positions.
At the same time, there are ways to make more money in sports medicine. There are all sorts of new injection therapies that are available for athletes. I don’t personally do a lot of those because I wanted to maintain a family medicine practice in addition to doing sports medicine.
Read Full Article on the DO: DOs at the Tokyo Olympics share the joys and challenges of working with world-class athletes
Simone Biles Withdrawal Puts Athletes’ Mental Health in Spotlight
Physicians attached to Olympic teams say they have been far more sensitive to athletes’ mental health needs during the pandemic.
Alex Myers, a physician for the U.S. rugby team who also works with college students and other athletes in San Diego, said she saw more generally an increase in phone calls regarding self-harm and suicide during the pandemic.
“Because of the pandemic, it ruptured the very frail social structures that a lot of young adults have,” Myers said. “Because of social media, every social interaction became more intense,” magnifying mental disorders that already existed and increasing the rate of emergence, she added.
Read Full Article on Bloomberg: Simone Biles Withdrawal Puts Athletes’ Mental Health in Spotlight

